|
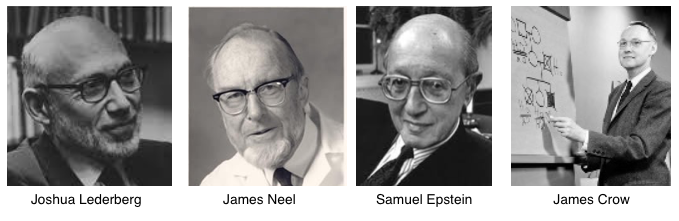
Were pioneering scientists who warned of a possible "genetic emergency" prescient geniuses or Chicken Littles? By Jill Escher Fifty years ago, around the time of the founding of the Environmental Mutagen Society (EMS), preeminent biologists, geneticists and toxicologists warned of a potential “genetic emergency.” This alarm referred to the possibility that exposures to novel chemicals and drugs flooding the market in the ebullient post-war era could be wreaking silent havoc in human germline, thereby weakening the developmental integrity of future generations. For example, in 1969 mutagenesis pioneer Sam Epstein warned, “At this moment we may be be in the midst of a potentially serious accidental experiment on the effects of chemical mutagens in man, the full impact of which may not be known for generations to come.” Nobel laureate Joshua Lederberg, knowing of germ cell vulnerability from animal models, in 1955 urged that “more extensive studies are needed to establish … whether germ cells of man are physiologically insulated against … chemical insults from the environment.” It was geneticist James Crow who in 1968 flat-out warned of chemicals causing a future “genetic emergency.” In “Chemical Risk to Future Generations,” he explained the possibility that “some compound presumed to be innocuous is in fact highly mutagenic and that large numbers are exposed before the danger is realized.” Were these men (and there were women, too, notably the mutagenesis researcher Charlotte Auerbach) and their colleagues prescient geniuses or Chicken Littles? (Fn 1) Have their fears about human germ cell damage come to pass? Or are our gametes so robustly resilient that the onslaught of post-war exposures bounced off them like so many ping pong balls? I think this is one of the greatest scientific and public health questions of our time. Clearly we aren’t seeing visible bad-movie-style mutants roaming our streets and crowding our schools. Cases of three-armed boys and seven-foot girls do not seem be on the rise. But what about more subtle, or at least less visible, phenotypes possibly resulting from mutated or otherwise damaged germ cells? Are we seeing an increase there? I would argue this is quite possibly the case. Over the past several decades we have seen staggering increases in somewhat invisible but often extravagantly disabling disorders of development, including autism, ADHD and learning disabilities. The prevalence of the paradigmatic of these pathologies, autism, has surged more than 20-fold in California since births in the 1980s, for example, and that’s counting only the more severe cases—now fueling a stupendous public health and social services crisis. It is frustrating, then, that autism causation research has been stuck in the dated paradigm of “genes” or “environment.” In the world of autism at least, the teachings of environmental mutagenesis (also referred to as genetic toxicology) seem to have fallen on deaf ears. The bulk of research funds have been spent on rather reductionist gene-hunting, with a lesser sum on potential impacts on fetal soma of environmental exposures, such as pregnancy drugs, adverse nutritional states, or pollutants. The idea that exogenous weird stuff could have damaged germline DNA or any of its many regulatory layers is barely on the radar. Certainly, the idea was barely mentioned during the 2017 International Meeting for Autism Research. At the same time, we are finding a plethora of heterogenous de novo mutations related to the condition. While researchers are quick to attribute these glitches to nothing more than random chance, I say not so fast. Autism is strongly heritable—among siblings. Yet there is essentially no evidence aside from some speculative statistical analyses that autism is handed down through the generations (such as this recent analysis by Wigler and colleagues). And these analytical approaches omit any potential role for exogenous perturbations of gene function; it’s as if the possibility never entered the minds of the researchers. But from a real-biology perspective there would be increased risk in siblings if at least one parent had suffered an adverse germline exposure, affecting genome, epigenome or cytoplasmic element such as mitochondria (ooocyte only), upping the risk for de novo heritable disease in multiple offspring. Strong heritability rates such as those seen in autism can not logically follow from random mutation, but rather from disruptions blanketing parental germ cells (and particularly, I would argue, early germ cells). Nevertheless, the possibility is seldom if ever discussed among geneticists. I would like to argue those doomsayers of the 1950s and 60s, those scientists who warned of a genetic emergency, may well have been prescient geniuses, and not Chicken Littles. Perhaps to a considerable extent today’s mysterious epidemics of neurodevelopmental pathology like autism have arisen as a consequence of silent damage in the human germline, inflicted by chemical forces thought at the time to be fairly innocuous (like, perhaps, my own fetal 1965 synthetic hormone drug exposures). Not ancestral “genes” alone. And not “environment” alone acting on fetal soma. While those single-dimension factors are of course important, why are we neglecting the founding EMS idea, now re-animated through the emerging field of germline epigenetics, that environment can alter our germline? This, I believe, is the forgotten realm of public health sciences. In our over-simplified approach, an entire dimension of biological risk has been neglected. This, I believe, is the forgotten realm of public health sciences. In our over-simplified approach, an entire dimension of biological risk has been neglected. Now, having been in the business for several years of identifying and funding opportunities to examine this outsider hypothesis, I am painfully aware of the difficulties inherent in generational, or germline, studies. In human cohorts, records of 1950s-1970s grandmaternal (F0) gestational exposures (such as to tobacco smoking or pharmaceutical drugs such as the soup of fake hormones to which I was prenatally exposed) are hard to find, and when they do exist, the records of grandchild (F2, sprung from exposed F1 fetal germline) may not be available. And then there are the confounds and complexities of any multigenerational study. Further, many tissues is of interest, including a mother’s eggs, are inaccessible. And a father’s sperm? There’s only been one study in that regard, and while it found differences in the autism father sperm methylome, it did not inquire into past exposures. In the animal model realm, developmental pathologies borne of early germline exposures are often readily seen, but people tend to question the applicability of those studies to humans. As autism epidemiologist Craig Newschaffer remarked to me, autism causation research "has a low-hanging fruit problem." And he's right. Why dig deep to look for old, forgotten exposures and 20 to 50 years of data, when you can simply write the umpteenth paper on paternal age (now that's low-hanging data)? As one epidemiologist remarked to me, autism causation research "has a low-hanging fruit problem." In spite of the logistical and analytical hurdles, germline exposure studies are certainly feasible, and in my view of course they must be done. The first study to be published on this issue relied on the rare trove of generational data of the ALSPAC cohort at University of Bristol in the UK. The study, funded by Escher Fund, found a link between grandmaternal pregnancy smoking and autism traits and diagnosed autism in grandchildren, through the exposed female parents (ie, early oocytes). While some journalists (for example here), found this link “baffling,” anyone cognizant of genetic toxicology would have little problem connecting plausible toxicological and biological dots. It's as if environmental mutagenesis has lapsed from the public consciousness. Fifty years ago mutagenesis was a young field. But today we have the benefit of many scientific insights that the pioneers could not have imagined. We now know, for example, that tobacco smoke is mutagenic. (Talk about something once presumed innocuous, I can only imagine the smoke-filled rooms of the early EMS meetings….). We know that synthetic hormone mimics, also known as endocrine disruptors, can exert adverse generational effects. We know of the importance of timing, and that primordial germ cells have heightened molecular vulnerabilities. And we increasingly know of multiple cellular mechanisms, well beyond classic exome mutations, that can exert heritable effects. This includes regulatory DNA, methylation and genomic imprinting, other epigenomic artifacts such as histone modifications and ncRNAs, and cytoplasmic structures such as mitochondria, and even possible receptor effects not touching DNA directly at all. DNA is but one piece of molecular heritability. "DNA is but one piece of molecular heritability." Given the tremendous advances in understanding early germ cell vulnerabilities (hey, and even late phases, too, as seen in this recent review of tobacco mutagenicity and adult phase sperm), I find it regrettable that public health research, and regulatory approaches as well, have overlooked this precious and powerful, if invisible, phase of the human lifecycle. There are few studies examining impacts of drugs or smoking on early germ cells, and regulatory approaches overlook them altogether. (Fn 2.) I do wish we will someday heed the words of those EMS pioneers, and geneticist James Neel, who in 1969 summed up what is at stake:
And what are we doing to protect, or even consider past exposures to, mankind's most vital asset? Well, today, I daresay, almost nothing. This is truly the forgotten realm of public health research. Notes: (1) EMS founders included Drs. Alexander Hollaender, Joshua Lederberg, James Crow, Ernst Freese, James Neel, William Russell, Heinrich Malling, Frederick J. de Serres, Matthew Meselson, among others. The EMS is now known by the name Environmental Mutagenesis and Genomics Society. (2) FDA risk assessment of pregnancy drugs, for example, omits any mention of potential impacts on fetal germline. This has been the subject of two Citizen Petitions filed by the Escher Fund for Autism. Jill Escher is the founder of the Escher Fund for Autism. In 1965 she was exposed in utero to continuous and heavy doses of synthetic steroid hormone drugs, a fact she discovered only in 2011. As the mother of two children with severe idiopathic autism, she has found many other affected families that share her exposure story, and has funded pilot research projects to examine possible associations between gestational toxicants, germ cell exposure, and adverse neurodevelopmental outcomes.
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorJill Escher, Escher Fund for Autism, is a California-based science philanthropist and mother of two children with severe autism, focused on the question of how environmentally induced germline disruptions may be contributing to today's epidemics of neurodevelopmental impairment. You can read about her discovery of her intensive prenatal exposure to synthetic hormone drugs here. Jill is also president of Autism Society San Francisco Bay Area. Archives
July 2021
Categories |
- Home
-
Expert Q&A
- Eva Jablonka Q&A
- Amander Clark Q&A
- Mirella Meyer-Ficca Q&A
- Janine LaSalle Q&A
- Dana Dolinoy Q&A
- Ben Laufer Q&A
- Tracy Bale Q&A
- Susan Murphy Q&A
- Alycia Halladay Q&A
- Wendy Chung Q&A
- Pradeep Bhide Q&A
- Pat Hunt Q&A
- Yauk and Marchetti Q&A
- Emilie Rissman Q&A
- Carol Kwiatkowski Q&A
- Linda Birnbaum Q&A
- Virender Rehan Q&A
- Carlos Guerrero-Bosagna Q&A
- Randy Jirtle Q&A
- Jerry Heindel Q&A
- Cheryl Walker Q&A
- Eileen McLaughlin Q&A
- Carmen Marsit Q&A
- Marisa Bartolomei Q&A
- Christopher Gregg Q&A
- Andrea Baccarelli Q&A
- David Moore Q&A
- Patrick Allard Q&A
- Catherine Dulac Q&A
- Lucas Argueso Q&A
- Toshi Shioda Q&A
- Miklos Toth Q&A
- Piroska Szabo Q&A
- Reinisch Q&A
- Klebanoff Q&A
- Denis Noble Q&A
- Germline in the News
- Science
- Presentations
- About Us
- Blog
Proudly powered by Weebly



 RSS Feed
RSS Feed